For most people, April Fools’ Day is a pretty harmless affair. What happened to Angela and Andrew Dower in Ocotillo Wells in 2023 was no practical joke.
“I do remember just waking u, and then hearing about what happened,” Andrew said. “And that’s a very bad feeling: of just learning about what happened to you.”
What Andrew doesn’t remember included multiple seizures and an emergency helicopter ride to the hospital. As an epileptic, seizures aren’t unusual for him, but the number he suffered that evening was.
“He kept seizing,” Angela told NBC 7. “He went to 3, 4, 5, 6. I knew something was wrong.”

After Angela called 911, park rangers and medics agreed with her assessment. Andrew needed to get to an emergency room. But even in an ambulance, a drive would take too long.
First responders called an air ambulance and sent Andrew to UC San Diego in La Jolla. There, doctors stabilized him and identified an aggressive brain tumor as the cause. Angela said that, within a month, he went under the knife.
A surprising denial from their insurance company
A different kind of scare came in the mail less than five months later from their health insurance company, Blue Shield of California.
“When we got the first denial, that was like putting an entire weight on your chest,” Angela said. “It was so, I guess, defiling to know that we pay our insurance rates, we do everything right, we go to the doctor and get our referrals. And then to know that they didn’t stand behind us in such a vulnerable moment and a very critical moment.”
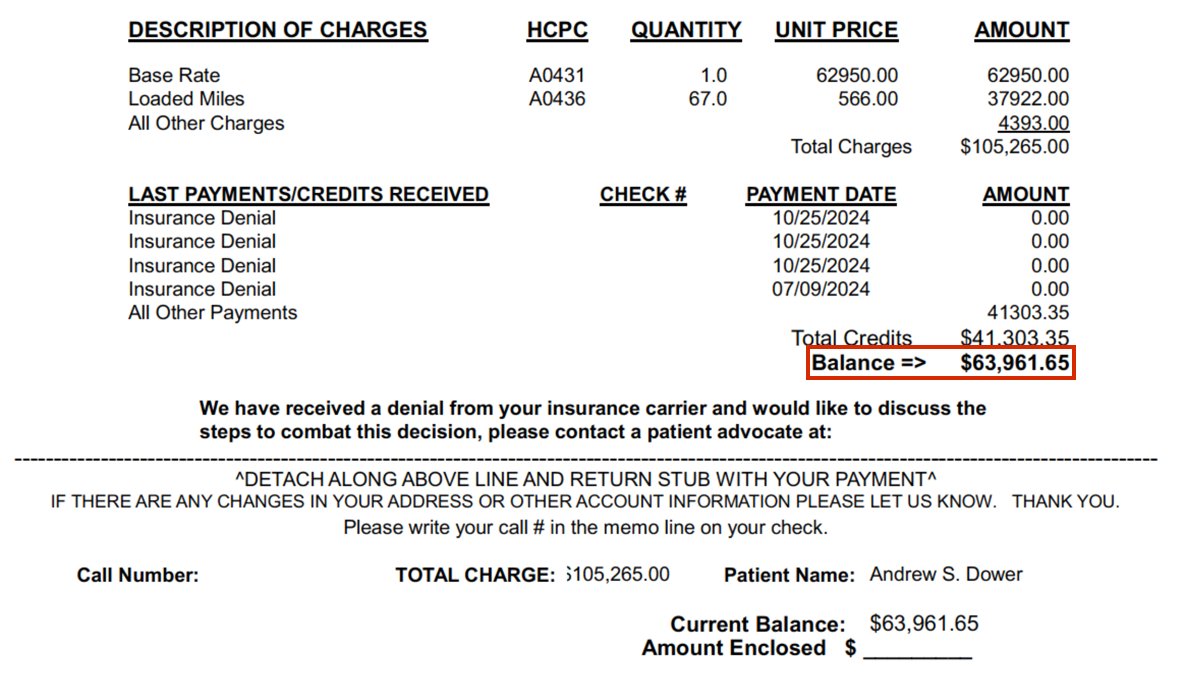
According to a letter from Blue Shield, the air ambulance wasn’t medically necessary and therefore wasn’t covered. That meant the Dowers were on the hook for nearly $64,000.
“If it wasn’t due to that air flight that day, he might not be sitting next to me right now,” Angela said. “That’s not what you want to hear. And to then hear that the insurance company just drops you and leaves you high and dry…. It makes you question everything. Why am I paying these bills? Why am I doing everything right?”
“Especially when the doctors were saying I was in status seizures, you could die, you were on the edge of death, essentially,” Andrew said.
According to the denial, Blue Shield determined the air ambulance wasn’t covered in part because it didn’t pick up Andrew at his “place of injury or illness.” The Dowers said their campsite was too rugged for the air ambulance to land, so a ground ambulance rushed Andrew to a nearby airstrip to get him to the air ambulance.
“To be told that you didn’t do the right thing when the doctors are all telling you you did the right thing — ‘you could have died here — that was hard to process,” Andrew said.
The family shared a document with NBC 7 Investigates from the flight crew that said the air ambulance was necessary, and that they took him to “the closest most appropriate facility.”
Denials became more common in recent years
Caitlin Donovan is senior director at the Patient Advocate Foundation, a nonprofit that helps people with serious diseases navigate the health care system.
“As soon as an air ambulance gets involved in a case, it should be a sign that the care is an emergency, immediate and necessary,” Donovan told NBC 7. “So it’s shocking to hear when it’s denied outright.”
Ever since the No Surprises Act of 2022 made it harder for health insurance companies to charge patients out-of-network rates, Donovan said, they’ve noticed providers increasingly resort to another workaround.
“Now instead of having to deal with that, they’re denying it outright,” Donovan said. “If you cover the hospital stay, the neurosurgery and not the air ambulance, there is no real explanation for it — other than they did not want to pay the high sticker price.”
NBC 7 Investigates asked the health insurer for answers

After Blue Shield of California denied two appeals, the Dowers asked the state of California for an independent medical review, but after what should have been a three-month process dragged on for nine, the family reached out to NBC 7 Investigates.
“Calling you guys was my last hope of desperation,” Angela said.
NBC 7’s team reached out to Blue Shield of California. A week and a half later, without explanation, the health insurer paid for Andrew’s air ambulance ride.
“For me, I cried,” Angela said. “I cried the minute that they told us. I felt that same weight that went on to my heart be lifted. I am forever grateful for you guys…. it was all thanks to you guys that we were able to expedite the closure of it and get it all paid.”
“We are in debt to NBC,” Andrew said.
Still, it’s hard for the relief to sink in after what the family went through.
“I spent countless hours, days on the phone, trying to get to the right department,” Angela said. “They would constantly tell me, ‘Oh, I’m sorry, they’re not in the office,’ ‘Oh, I’m sorry they can’t speak,’ ‘Oh, I’m sorry that’s just the way it is.’ And it took you guys to get to the right department. And that’s just disheartening to me. It’s disappointing to me that it has to be that hard.”
Blue Shield told us they couldn’t comment because of privacy reasons. In the past, our team has talked to insurance companies after patients sign a privacy waiver. We asked Blue Shield three times for that waiver so they could speak openly about this case, but Blue Shield ignored us each time.
Angela wants more than just answers.
“I would love an apology, honestly, for interfering and causing so much unnecessary stress and worry, and hardship on our family and loopholes and things we had to jump through,” Angela said. “Why does it have to be this hard?”
“The scale of the story and how obviously in the wrong the insurance company was makes it shocking,” Donovan said. “What’s not shocking is that a patient’s care is being denied to save the industry money.”
How to fight back after a health claim is denied
You can get help from the Patient Advocate Foundation if you believe your health insurance wrongly denied a claim. On its website, you can find templates for how to appeal.
The state also wouldn’t comment on Andrew’s case, but NBC 7 Investigates found there’s a chance of getting a denial reversed.
Since 2017, the California’s Independent Medical Review program looked at 32 cases involving emergency transportation. In about two-thirds of those cases, 21, the state overturned the decision from the health plan.

Want more insights? Join Working Title - our career elevating newsletter and get the future of work delivered weekly.